Tobi Maracle was taking her oldest child to the Child and Family Developmental Services even before it opened a new clinic in the Alaska Native Medical Center in Anchorage.
By the time the child was 5 years old, they were visiting three times a week for speech and occupational therapy. A months-long wait for applied behavioral services was ending, and they were excited by the progress.
Then the pandemic came and everything stopped.
Maracle, the mother of three children in an Anishinaabe-Mohawk family, wasn’t sure what would happen next.
Within a few weeks, however, her phone rang. The healthcare workers were ready to run their sessions online. They assembled kits with the needed materials and dropped them by the house.

Courtesy of Tobi Maracle
Therapists at the Alaska Native Medical Center in Anchorage, Alaska, were able to adapt lessons to telehealth services during the pandemic, helping children and caregivers alike continue receiving services. Tobi Maracle, the mother of three children in an Anishinaabe-Mohawk family, says the use of telehealth services has given her family more time to be together.
Maracle watched as the occupational therapist modified handwriting lessons in imaginative ways, making the most of the technology. She was surprised how fast her 5-year-old adapted to this new way of working with both the occupational therapist and speech-language pathologist online, she said.
“He loved the interaction,” Maracle said. “You could see how sad he was when it ended.”
The recent growth in telehealth is bringing new options to remote Indigenous communities for people with developmental needs such as autism and their families, who often live far from services. The pandemic has spurred more providers and clients to try telehealth as a way to connect and has triggered new research into autism services via telehealth.
A recent study of services in Iceland found that parents could learn and retain the skills that they need to better support a child with autism, and demonstrated that it is also possible to communicate securely and effectively on an older, wireless network.
“There is increased attention to understanding how to make it most effective, and how to overcome the difficulties, and capitalize on strengths offered by technologies,” said Shahla Ala’i-Rosales, co-author of the study.
Building on a legacy
Delivering health services by phone or videoconference has been operating in Indian Country for decades. The Indian Health Service first delivered telehealth services to the Tohono O’odham Nation in Arizona in 1973 through a partnership with NASA and Lockheed Martin.
The IHS telehealth system expanded with the onslaught of COVID-19 in 2020, increasing from an average of 1,300 a month pre-COVID to more than 41,000 per month at the height of the pandemic. The average as of October 2022 was about 11,000 telehealth visits per month, according to IHS.
And in early November, IHS announced further expansion of its telehealth services after awarding a contract to AA RingMD, a cloud-based program that provides a secure system for telehealth conferences.
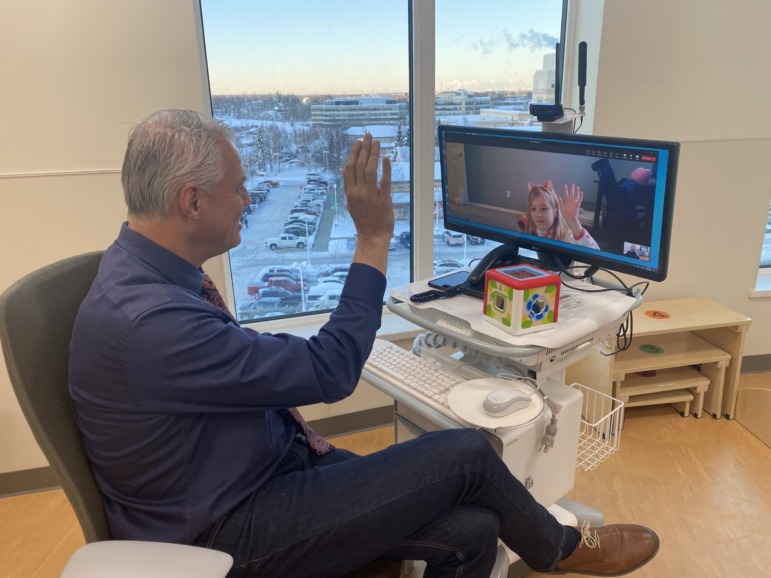
Courtesy of the Alaska Native Tribal Health Consortium
Dr. Randall Zernzach, a developmental pediatrician with the Alaska Native Tribal Health Consortium, uses telehealth to work with a young patient on Dec. 9, 2022. The use of telemedicine is expanding options for families who may not have easy access to treatment.
“This expansion of telehealth will increase access to care, patient safety, continuity of care, quality of care, and ultimately patient satisfaction,” said IHS Director Roselyn Tso, Diné, the first Indigenous person to head the service. “We look forward to being able to reach even more of our American Indian and Alaska Native patients across Indian Country.”
Alaska’s tribal health system, the Alaska Native Tribal Health Consortium, has emerged as a leader in telemedicine. The tribal system serves more than 100,000 Alaska Natives, most of whom live in small communities with limited road access that is further hampered by weather, terrain and demographics.
The consortium has provided equipment, software and technical support since 1998, now reaching 44 health care providers serving 248 sites in Alaska.
Dr. Randall Zernzach, a developmental pediatrician, said the new building at the Alaska Native Medical Center opened in 2018 with the capability to deliver services through videoconferencing. Aside from a few therapists who were early adopters, the rest of the clinic staff moved slowly to use the option. He called himself “a good soldier” in trying to use it himself.
But the entire staff pivoted after the pandemic took hold and they couldn’t see clients in person.
“This can’t go on,” he recalled saying after the first week of the lockdown. “We are trying to help an entire state.”
Over time, he and the other providers saw that the technology could foster connections. For example, when a medical team visited with families during the lockdown, everyone’s home was in the background on Zoom, making it look like the Brady Bunch, he said.
“You could have the conversation and hear the story from their own dining room,” he said.
New approaches
For Maracle and other families facing autism, telehealth can provide new ways of addressing their needs while saving time.
Parents and caregivers are sometimes surprised to learn about the wide range of services an autistic child might need, said Candi Running Bear, Navajo, who is on hiatus as a special education teacher to work on a project at the University of Northern Arizona that connects autism families to the help they need.
Running Bear, who is also working with a new Navajo Nation program on autism, said the needed services can include physical, occupational, and speech therapy as well as parent training and interventions based on applied behavior analysis, such as learning to use the toilet.
With the right information and support, parents and caregivers can better assist their child in learning to communicate and imitate others, she said.
Children with autism often have trouble mastering those two basic skills, which are needed for learning how to learn. But once they are better able to communicate and learn from imitation, a child’s choices for school and community life can greatly expand, especially when they have support from their extended family, friends and neighbors.
Without telehealth options, some families leave home and community behind to access services — a decision that would tax any family’s resources but can also tax a family’s resilience.
Some children make more progress when services are delivered in person, especially when integrated into the school day, she said. But parents and teachers also recognize the need for access to experienced providers.
“For access to services from people who are knowledgeable, sometimes you can only get that through telehealth,” she said.
Telehealth services can also be added to in-person services. Sometimes providers must first build rapport by working one-on-one with a child, experts say.
Regan Garden, a clinical director with MethodWorks in Alaska, said a therapist might need three days to travel, in the best conditions, to reach a child in a remote community. Connecting by phone or video between those in-person visits can help therapists manage travel time and serve as many children and families as possible.
But it’s not a fit for everyone. Some children may not respond well to therapists on a videoconference, but telehealth still provides a way of training parents, caregivers, teachers and other people around the child.
Research shows that children progress faster, and more sustainably, when the people around them are building their own knowledge and skills. That can often mean putting a camera in the home, classroom or clinic, to allow consultants to observe and then help caregivers adjust their responses so small problems don’t become full-blown crises.
For example, if a child is having trouble communicating their preferences to the people around them, they might become aggressive toward others or develop a self-injurious behavior without expert help.
“You can watch a lot,” said Mychal Machado, a psychology professor at the University of Alaska who has assisted families in crisis. “But it can feel like ‘Big Brother.’”
Training can feel less intrusive if the help on the other side of the camera is culturally competent. Just before the pandemic took hold, Olivia Lindly, a public health professor and researcher at Northern Arizona University, received funding to support a new autism program in the Navajo Nation.
The program, Parents Taking Action, was developed about 12 years ago for Latino families in Texas. The program has sturdy guidelines for adapting any research-based materials to cultural needs, and has been expanded to include Chinese immigrant families in Chicago and Black families in Baltimore, Lindly said.
The Navajo iteration of Parents Taking Action connects information and services to those who benefit, similar to the community health network that is delivering diabetes education and other health programs, Lindly said. When the pandemic hit, Lindly and others adapted the parent program for virtual delivery.
After the Navajo Nation’s local chapters approved the project, the program trained five caregivers for children with autism, ages 4-15. Now, those five people are helping train 10 more families of children from 2-12 years old, Lindly said. Running Bear is among those working on the program.
The process has been intensive, but should be sustainable, Lindly said.
“It does fill a gap in services,” she said.
‘A better experience’
As travel restrictions from the pandemic eased, health care providers realized anew how difficult it can be on families to travel to a clinic for services.
At the Alaska Native Medical Center, services are exceeding pre-pandemic levels as the teams blend in-person and telehealth delivery, Zernzach said. Staff can get the ball rolling for new families without asking them to fly in right away, or by making follow-up visits and managing a system of care through telehealth, he said.
“It makes for a better experience,” Zernzach said.
Maracle said that while her family lives close to providers in Anchorage, telehealth gives her more options while saving time and energy.
“I’m not loading up the car and on the road for two hours every day,” she said.
Recently, Zernzach recommended that her middle child also receive services. This time, however, telehealth was not a good option for delivering therapy and other direct services.
“He wants nothing to do with it,” she said.
Instead, Maracle leaned into the many parent-training options offered online, which she found rewarding.
“I was getting coached on why we were doing what we were doing,” Maracle said. “I was in the driver’s seat.
***
Peggy Heinkel-Wolfe, who is non-Native, is an independent journalist based in Texas and the co-author of a new book with Shahla Ala’i-Rosales, “Responsible and Responsive Parenting in Autism: Between Now and Dreams.” Her previous book, “See Sam Run, a mother’s memoir of autism,” received the Mayborn Nonfiction Prize in 2005.































