Kaylee Joaquim is stretched out on the couch, surrounded by remnants of her old life. Softball memorabilia line the entranceway of her family’s suburban Boston home. Sports trophies fight for space with certificates of achievement and art projects on the shelves.
Instead of pitching at softball tournaments, the 13-year-old has spent days in this position since she contracted COVID-19 in January 2022.

Kaelyn Lynch/For Youth Today
A softball sits outside the suburban Boston home of Kaylee Joaquim.
“She used to be on the softball field six days a week before this,” her mom, Andrea Joaquim, said. “Now she’s on the field for 15 minutes every three months.”
Kaylee is one of hundreds of thousands of children and teens living with long COVID, defined as lingering or new symptoms after a COVID-19 infection that can last for months or years. Their widely varied symptoms — from rashes and trouble remembering things to excruciating limb and stomach pain and weight loss — have resulted in some youth failing academically, dropping out and delaying college. Others have had to fight for accommodations, including the right to remote instruction and not having to take the stairs to class.
“Watching the kid who used to bounce around everywhere lay sedentary for days at a time is heartbreaking,” Andrea Joaquim said. “I’d love to see her be a normal 13-year-old, but this isn’t it.”
Long COVID is hard to track. Research estimates that anywhere from 4% to 25% of the 15.6 million American children and adolescents who have had a COVID-19 infection will develop some form of long COVID.
In kids as in adults, there are no known cures and few effective treatments.In a nationwide study of long COVID in adults, published in JAMA in May 2023, researchers at major medical universities and Massachusetts General Hospital found that the most common symptoms are post-exertional malaise (a significant worsening of symptoms, or development of new ones, after minor physical or mental effort), fatigue, dizziness, heart palpitations, brain fog and gastrointestinal issues.
“The most common complaints we see are profound fatigue that interferes with daily life, post-exertional fatigue and brain fog,” said Victoria Brown, a social worker with Boston Children’s Hospital’s pediatric post-COVID clinic. She said that about 75% of the kids that come into the long COVID clinic are generally healthy, have no preexisting conditions and have seen their lives significantly affected.
[Help us report on long COVID in kids]
Long COVID and the struggle to access care
Nineteen-year-old Haley Nelson from New Jersey is a self-described high-achiever who thrives under pressure. She was the captain of her varsity tennis team, a leader on student council and a straight-As “perfectionist” with plans to attend Boston College. After contracting COVID-19, she developed a constellation of symptoms: dizziness and fainting spells on the tennis court, leadened limbs that were hard to move in the morning and brain fog while reading. The more she pushed through her symptoms, the worse she got.
A neurologist, recommended by a family friend, suggested her symptoms were caused by anxiety and stress. She referred Nelson to a psychiatric hospital. “I felt so disbelieved, like she was not acknowledging me at all,” Nelson said. Later, reviewing notes from the appointment, Nelson noticed the doctor had not written down any of her physical symptoms.
“When doctors don’t know the reason for chronic conditions, the psychological excuse is always an escape option,” said Dr. Danilo Buonsenso, a physician at Gemelli University Hospital in Rome who treats and studies kids with long COVID. “That’s particularly true for kids and adolescents.”
Sammie McFarland, the founder of U.K.-based charity Long COVID Kids, said that attitude is fueling diagnoses of functional neurological disorders, a blanket term that suggests psychological problems are causing physical symptoms. “You get that diagnosis and it’s like you’ve fallen off the planet,” McFarland said, “There’s no further support, no ongoing tests, no review process.”
Brown, the Boston Children’s social worker, noted that the hospital provides psychological support, including counseling for patients and their families, and acknowledged that mental health is a component of the illness, but not at its root.
“The reason we check in about mental health and mood is not because we think that’s a primary component, but we know physical symptoms can be really tough to deal with,” she said. ”That’s why we ask about it and recommend support.”

Kaelyn Lynch/For Youth Today
Kaylee Joaquim uses an iPad at her suburban Boston home.
The American Academy of Pediatrics’ guidelines on pediatric long COVID recommend a team-based approach of specialists, headed by a primary care physician, to coordinate testing and treat patients’ worst symptoms. But patients often do not receive that level of care.
Allison Hinkler, of Ohio, said that her 13-year-old daughter Anna Hinkler’s long COVID symptoms — including stomach pain so severe she could no longer eat, dropping her five-foot-nine frame to 112 pounds — were dismissed as mental or behavioral health issues by her pediatrician.
“They drug tested my 13-year-old without my consent,” she said.
It took three more visits for her daughter to be referred to specialists but, her mother said, getting them to order additional testing or try new treatments was a challenge. “They say, ‘long COVID is a mystery and there’s nothing we can do to help you,’” Hinkler said.
As a result, Hinkler, a high school science teacher with a masters’ degree in biology has had to become an advocate for her kid.
“I wake up at 4:30 in the morning to do research and develop a list of things to talk to each specialist about,” Hinkler said.
Dozens of specialty long COVID clinics have sprouted up across America but, currently, just 14 treat people under 18, and many have months-long waiting lists. That leads some parents to travel far from home and pay out-of-pocket for treatment.
After a February 2021 COVID infection, Rochelle Rankin’s then 15-year-old daughter Katie developed fatigue, pain and gastrointestinal symptoms so severe that she sometimes could not even lift her phone. After their Las Vegas pediatrician dismissed Katie’s symptoms, Rankin took her daughter from Nevada to San Diego to see a physician who specializes in long COVID care.The cardiologist picked up on anomalies in Katie’s heart that routine tests had missed. One of Katie’s original doctors thanked Rankin later, saying that the research she sent had helped him recognize and treat long COVID in other young patients, Rankin said. “But that’s not my job as a parent,” Rankin said, recalling her thoughts. “That’s yours as a doctor.”
Part of the problem is a lack of clinically validated treatments. There have been few treatment trials for long COVID in adults and even fewer for kids.
“We’re a little more cautious on doing research in children because you’re reliant on a proxy, in other words, their caregivers, to give consent,” said Dr. Laura Malone, a pediatric neurologist and co-director of the Kennedy Krieger Institute’s Pediatric Post-COVID-19 Rehabilitation Clinic. “A lot of research is done more commonly in adults and then in a second level it can occur in children and adolescents.”
Money is another problem. “Pediatric long COVID is specifically underfunded,” said Buonsenso, the Italy-based physician treating and researching kids with long COVID.
In the meantime, some parents say they find themselves lugging binders of medical records and research papers to doctors’ appointments.
“I’d like to see doctors think more outside-the-box,” Rankin said. “I’ve got a 17-year-old who can’t walk down the stairs. I can’t wait for science to catch up.”
[Help us report on long COVID in kids]
Long COVID and trouble at school
In addition to being a softball star, pitching no-hitters and playing as many as six games a weekend at tournaments, Kaylee Joaquim was one of the top students in her grade, earning As in every class.
“She was a sponge,” her mother said. “You’d tell her something and she’d remember every single detail of what you said. Now, you ask her to remember five things, and an hour later she won’t even remember having the conversation with you.” Kaylee’s fatigue made it hard to attend class. Averaging two and a half days per week of school attendance, her grades dropped to Cs and Ds.
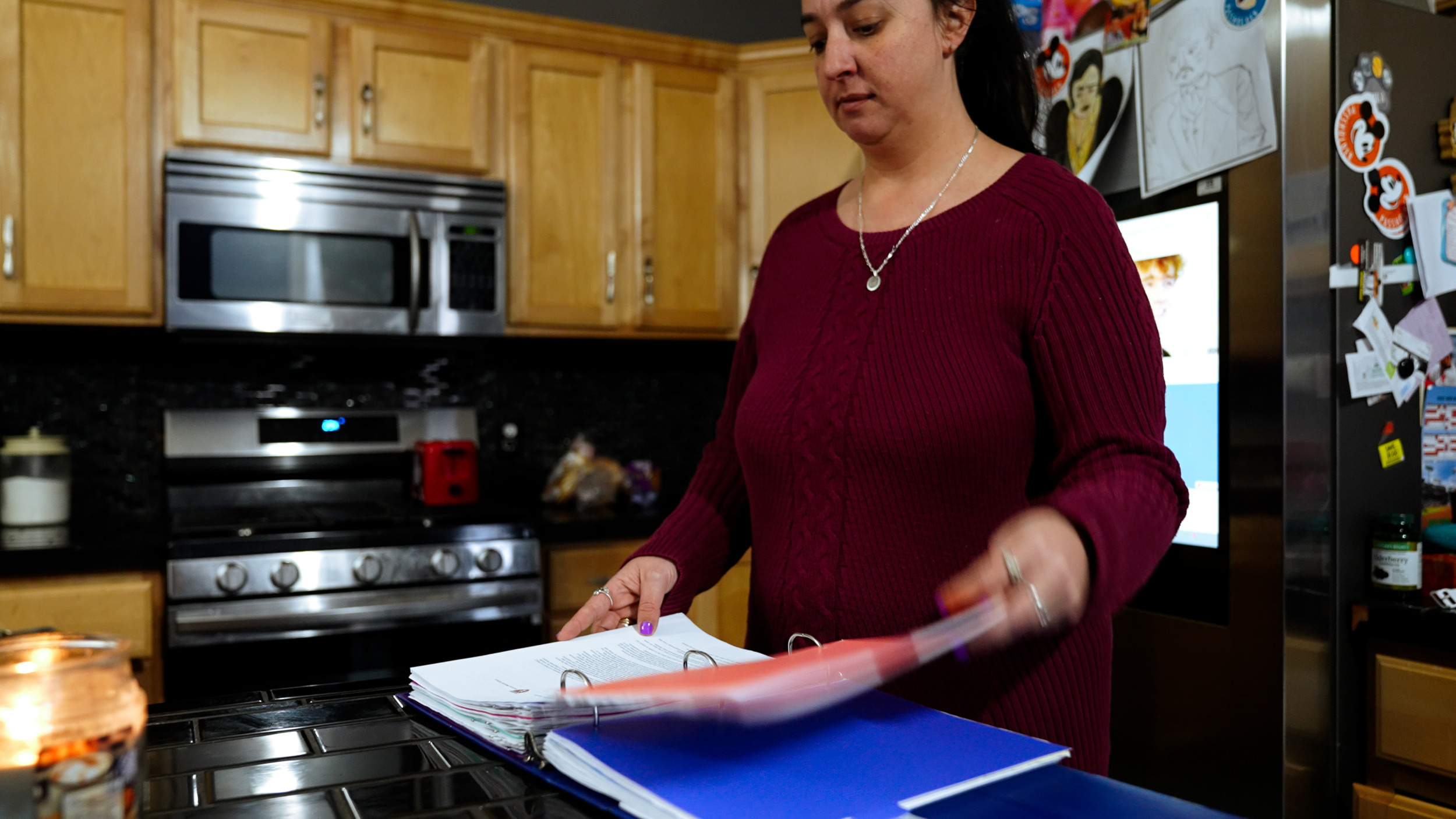
Kaelyn Lynch/For Youth Today
Andrea Joaquim looks at a binder of her daughter’s long COVID medical records at their suburban Boston home.
In guidelines released in July 2021, the U.S. Department of Education said that students with long COVID are protected under Section 504 of the Rehabilitation Act of 1973 and the Individuals with Disabilities Education Act, which require that public schools accommodate kids with disabilities. Brown, the Boston Children’s social worker, works with schools to develop and implement Section 504 plans and said this can mean things like extra time for tests, more excused medical absences, remote classes and teachers sharing copies of lessons.
While public schools are legally required to accommodate 504 plans, Kaylee Joaquim said hers was not implemented effectively. She was given an elevator key, but often had to take the stairs. And her school suggested that her many absences might mean she’d have to repeat the 7th grade. The Rockland school district did not return calls seeking comment.
“Taking the stairs would have her on the couch for three days,” her mother said. “I would physically have to carry her into school some days.”
Getting any school — public or private — to believe long COVID is a real disability in the first place can be a challenge.
Anna Hinkler said her teachers at her private school only started believing her and offering help after she got a feeding tube to help with gastroparesis, a paralysis of the stomach muscles, that now drips a protein shake into her stomach overnight. Once she had to go to school with the feeding plastic tube taped to her face, “They started thinking, ‘Oh, this really must be physical,’” Alison Hinkler said. “Because who would want this?”
Georgia Treadway, a 16-year-old with long COVID from Oregon, said her day-to-day functioning is unpredictable. She spent over six months following a COVID infection in late 2021 entirely in bed, barely able to attend school. She recovered somewhat over the summer, but would relapse when she tried to go back to classes.
“Just because I’m fine one day doesn’t mean I’m better,” Treadway said. “It means I’ve saved up enough energy to act normal for a short time.” Her school told her she had missed too many days to graduate. This past spring, she dropped out, and is now pursuing a GED diploma.
If schools are not implementing 504 plans, parents have the legal right to demand one by working directly with school administrators or through a mediator. They also can request an impartial hearing or file a dispute with the federal Department of Education. But resolutions can take months or years.
With a letter to her school from Boston Children’s, Kaylee was able to move to fully remote classes. “We noticed she was getting good grades when she was here but, when she had to go to school and be in pain all day, her grades would plummet,” her mother said.
[Help us report on long COVID in kids]
Long COVID’s altered futures
According to a review of 40 studies, about 10% of kids with long COVID have since reported resolution of all of their symptoms, but for many young patients, their lives have already been irrevocably changed.
“There are some patients that we see that are high-achieving athletes and maybe they can’t do that anymore, but they can still go to school,” Malone, the physician at Kennedy Krieger Institute, said.
Boston Children’s Brown said that, with treatment, most of her patients do improve. She has seen both partial and full recoveries on varying timelines between six to 18 months.
Even without a full recovery, proper medical care can make a difference. Kaylee saw improvements in her memory after doing occupational therapy similar to post-concussion treatment.
Katie, who had 25 absences in a four-month school semester, has not missed a single day since she was diagnosed with a childhood version of fibromyalgia — whose symptoms include intense physical pain throughout the body — and started an intensive rehabilitation program. She now plans to attend college in the fall.
Anna Hinkler regained weight after getting a feeding tube and her fatigue lessened after doctors at the University Hospital Rainbow Babies and Childrens’ long COVID program in Cleveland took an integrative approach to her treatment. There, multiple physicians worked together as a team to look at how symptoms manifested across different systems in her body and tried new medications.
Georgia Treadway slowly began to exercise again; medications prescribed to treat postural orthostatic tachycardia syndrome improved her heart palpitations and fatigue.
Haley Nelson continues to struggle, but she finished high school and was determined to start college last fall. However, she collapsed on the floor shortly after moving into her dorm. She made it to one class, which she said she “loved more than anything,” but felt dizzy and couldn’t focus on the lecture due to brain fog. She decided to return home.
“It was one of the hardest things I’ve ever had to do,” she said. “I felt like a failure in so many ways.”
Now, she spends much of her time resting and bouncing between doctors’ appointments.
“I look out my window on the days I can’t function and see everything I’ve wanted to do, watching the world go by,” she said. “Whatever I say isn’t going to capture how painful it is, physically and emotionally, to not see an end.”
***
Kaelyn Lynch is a New York City-based multimedia journalist.
***
Help us report on long COVID in kids
🧒 Are you a young person who has or had long COVID?
🏡 Are you a parent of or caregiver for a pediatric long COVID patient?
🚑 Do you deal with pediatric long COVID as a medical or insurance professional, researcher or educator?
📢 We want to hear from you.
***






























