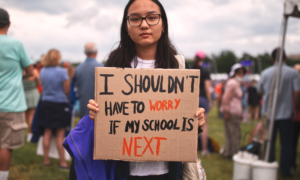
Photographee.eu/Shutterstock
From training to practicing to now teaching, one of the key factors in psychotherapy that continually surfaces is countertransference (sorry self-care), which we know as the phenomenon of the clinician reaction to the client. I prefer to think of countertransference as our “entanglement” with the client — it is never neat and organized. And I think a lot of managing entanglement starts with recognizing that fundamentally, clinicians are entangled with themselves and the stories we create for ourselves. So this is a story about the story about my entanglements.
I began working as a behavioral health clinician in a juvenile detention center mainly by chance, so the experience was going to be completely new to me. I had no prior training with this population, and while I did have experience in a residential setting, the idea of going to do behavioral therapy in a secure detention center was an unknown for me.

Sean E. Snyder
So my clinician story started with projection and preconception. The overt preconceptions are easy to see going into the detention setting — these youth are here for allegations of violent offenses, property crimes, drug-related crimes. My introduction to providing care in this setting was reassurances from the organization in charge: that the detention staff will be outside the door in case something happens, or if a youth is on what is known as “one-to-one” supervision, staff could come into the room during the session.
I saw my first youth for needs assessment and the encounter remains unforgettable. Here is this adolescent in blue scrubs, no identifiable features, and I knew nothing. Admittedly, it felt like I was getting through sessions as quickly as possible because I didn’t really know what to do. There was that first-session anxiety — the functional kind in new scenarios — but I remember trying to resist the preconceptions and projections.
Cue overcompensation. To resolve my “quickness,” my story came to involve seeing as many youth as possible to extend my reach, to build a sense of competence with me, to try to provide the most access for what seemed to be a scarce resource. But I resisted getting entangled with the depth of their stories, and looking back, it seems largely protective of my story.
Reality always wins. As months became a year and beyond, I struggled with the youth readmissions and recidivism, questioning myself: “Why were they coming back so frequently? What role did I have to play in this?” Clinicians tend to overstate their importance and downplay their role in undesirable outcomes (anecdotally and empirically speaking …), and so I figured this must just be a total product of the flawed system. The system wasn’t trauma-informed, not responsive to the needs of adolescents in a large urban area. So the rescue fantasy, the fantasy where a “helper” will save vulnerable people from their plight, came in full force.
Nothing works with everyone
After establishing my workflow and processes, I was fortunate to be trained in trauma-focused cognitive behavioral therapy, the key (in my mind) that would unlock the system and produce such good outcomes. At the time, this training felt like the panacea that I had been looking for. With all of the trauma exposure these youth experience, clearly the answer to their challenges was trauma-focused treatment. I had my daily musings: “If I could just get youth to do this treatment, then the likelihood of their return should decrease.”
I did have some treatment success, even with small doses of the intervention, but I generalized the model to practically every youth that I saw. To take a step back, there is no doubt that youth can benefit from skill-building interventions and some exposure to their stressors, but with my practice, I went a little overboard. I was defining my story further by negotiating how I would get entangled with my clients — I’d go by what the evidence says. And I was not ready for the impact of the entanglement of trauma work.
By putting myself out there with trauma treatment, I wasn’t ready for the effects of it. The fatigue was something I rationalized. Month by month, I began developing burnout symptoms and eventually I had secondary traumatic stress symptoms. I superficially sensed that I needed to go to therapy but I was so reluctant because it didn’t fit my story. I had chosen to do this work and it was just the byproduct of my decision. And I told myself, “I will press on and get through it.” ( I did eventually go for my own therapy.).
The story kept going because I had been doing the treatment and there were enough results, albeit mixed results. Some youth were getting “better” with their symptoms, some got worse, some I never saw again. Then there were some who appeared so much more functionally present but still reported high levels of symptoms. Here was the new challenge I had to overcome — “incongruence.”
I began to get crazy about measurement-based care, thinking “if I just measured everything correctly, then I would be able to get the results I was hoping for.” Stop me if you have heard this — treatment becoming more about the clinician’s insecurity than the patient’s needs. (For reference, our team systematically used the PHQ-9, GAD-7, the Mood and Feelings Questionnaire, the Peabody Treatment Progress Battery, the Childhood PTSD Symptom Scale-5 and the Columbia Suicide Severity Rating Scale.)
I did my new and improved measurements, and some of these activities helped. I incorporated the CGI scale to give myself some slack about functional improvement but lack of symptom reduction. As an aside, this part of my story is not to trash measurement-based care; it is a really effective practice for client treatment outcomes. But it was another way for me to keep the reins on my story, to manage the entanglement.
In my craze of figuring out measurement, I got connected to a brilliant doctor/researcher on the West Coast who was doing amazing work with pain management in children. She gave me what I was looking for with notes about measures, problem hierarchies; but she gave me something so much more at the end of that email: “Have you ever heard of healing-centered engagement?”
That question challenged the story, and I can see that she engaged my head to get at the heart of what the work is all about. The youth aren’t their traumas, they are more than just what happened to them and their collection of experiences.
Shut up and listen
Thomas Merton, a social activist of the 1960s and American Trappist monk, mentioned in his “Letter to a Young Activist” that the work becomes less about the problem and more about the people. More eloquently put:
“Do not depend on the hope of results. You may have to face the fact that your work will be apparently worthless and even achieve no result at all, if not perhaps results opposite to what you expect. As you get used to this idea, you start more and more to concentrate not on the results, but on the value, the rightness, the truth of the work itself. You gradually struggle less and less for an idea and more and more for specific people. In the end, it is the reality of personal relationships that saves everything.”
Sometimes, to get the message, you really have to shut up and start listening more as a clinician. For years, I told everyone who asks about my work that the best part of the job is the people, the youth I am honored to see. I get the chance to grow alongside them, to have moments of grace, shared joys and shared disappointments. I’ve seen some youth grow up in the system, and while that is disheartening, they are still people under our care. So the story now becomes less about symptom reduction, measurements, congruence and my story, and it becomes more about what all this means for them, how their identity and self-concept are affected, how they are striving toward the self that they envision for themselves.
Then there are those wake-up call moments that really put things into perspective. I have learned of the deaths of many youths I had clinical contact with, with cause of death ranging from intentional or unintentional shootings to suicide to unintentional overdose. My initial reaction to the first client death was another fantasy: “How did I not delay death for this youth.”
It is a complete shock to hear a client has died, as it really is the most existential entanglement possible. And it’s moments like these that really make me think back to why I do this work in the first place — to improve the quality of life of people and their communities. It’s going back to that mission, the mission of healing, of resilience, of striving towards the possible, that helps to keep me moving forward. It’s about their stories and my stories together at this instance of time. Social work is not about delaying death but enhancing life. It’s authoring the story for what it is, what it could be, the mess, entanglements and everything in between.
Sean Snyder, MSW, LCSW is a licensed clinical worker practicing and teaching in Philadelphia. He enjoys Phillies baseball.