This story was originally published by MindSite News.
![]()
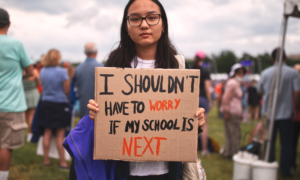
‘Bad kid’ diagnosis ‘greases the school-to-prison pipeline,’ doctor says ![]()
Black children are disproportionately diagnosed with a mental health condition known as oppositional defiant disorder (ODD), which serves to label them as “bad kids” and perpetuates systemic racism, says a California psychiatrist in a new report released this month.
As explained by the Mayo Clinic, ODD includes a frequent and ongoing pattern of anger, irritability, arguing and defiance toward parents and other authority figures. ODD also includes being spiteful and seeking revenge, a behavior called vindictiveness.
Amina Touray/Courtesy Dr. Legha
Dr. Rupi Legha is a California-based child psychiatrist offering anti-racist solutions.
“I often say ODD greases the school-to-prison pipeline,” Dr. Rupi Legha, a Los Angeles-based child and adolescent psychiatrist, told MindSite News. “It becomes a way to shove kids quicker. They’re going to slip and fall a lot more and it’s going to go a lot faster.”
Legha calls herself the “antiracist MD.”
A 2024 paper published in Scientific Reports found that the diagnosis is 35% more prevalent in Black people than white people and, more alarmingly, that conduct disorders – a group of behavioral conditions that includes ODD – is diagnosed more than twice as often in Black children and 73% more often in Black adolescents, compared with white youth. Legha’s report about the overdiagnosis of the disorder and what psychiatrists can do to disrupt the pipeline was published in the journal of the American Academy of Pediatrics.
Legha calls herself the “antiracist MD.” She has created an “antiracist solution” that provides a framework for providers that links ODD to the legacy of racism, documents systemic inequities and advocates for trauma-informed care that rehumanizes children.
The interview
MindSite News spoke with Legha about her approach. This conversation has been edited for brevity and clarity.
Josh McGhee: What does it mean to take an anti-racist approach to mental health disorders?
Dr. Legha: What it means for mental health disorders and health care more broadly is to be deeply aware of the inequities that are shaping care and to understand and trace the historical arcs giving rise to them. Then you need to have very key strategies related to what you’re doing in the moment as a clinician-researcher while also thinking about broader policies and practices that go beyond that immediate moment that you’re in.
What drew your interest to Oppositional Defiant Disorder?
I’m a child psychiatrist. From fellowship training and working in different county mental health settings, whether it’s emergency rooms, or outpatient clinics, it’s hard to not notice the pattern of seeing primarily Black, but also brown children showing up with an Oppositional Defiant Disorder diagnosis. As a new child psychiatrist, that pattern was apparent immediately and the research backs up that it is overdiagnosed in minority kids. That was coming up a lot so it was something that I had to tune into.
My oath was to take care of and protect these kids. Usually, it’s maintaining the standard of care for them, but what I quickly realized was that in order to enact that oath, I had to pivot to something else. And that something else was not apparent. It was not like supervisors were giving that to me. It’s not like there were new standards coming out to teach me. It really was me figuring it out through my heart and mind what I needed to do to be a child mental health therapist better protecting these kids.
Why is it important to take an antiracist approach?
It becomes a ‘bad kid’ label for marginalized kids of different ethnicities, but there’s something about the racialized nature of it that is particularly important. If you look at the history of the diagnosis or the history of diagnostic condemnation, as I call it, it is very tied to an anti-Black sentiment related to slavery and its aftermath.
I will often say that Oppositional Defiant Disorder is the 21st-century version of drapetomania. Drapetomania was this “diagnosis” during the 19th century that a psychiatrist named Samuel Cartwright came up with. Drapetomania was runaway slave syndrome and the treatment for it was whipping. Very early on, you see this racialized approach to diagnostic practices and the ways in which they perpetuate racism.
Why does this classification lead to stricter disciplinary action instead of solutions?
Like other diagnostic labels, it’s a form of judgment. It’s a label that gets placed on a child and it becomes an instrument perpetuating coercion and force. What I often see is that punitive or harsher disciplinary or even treatment interventions become an option of convenience instead of an option of last resort.
[Related Report: Redesigning the health care delivery system to better meet the needs of youth]
In the emergency room settings, you will see the ODD label serving as a conduit towards seclusion and restraint — a kid that needs to be tied down. In an outpatient setting, you’re not going to see kids restrained or tied down, but discipline and parent training are coming up. In school settings, you’re going to see suspension and expulsion. In juvenile justice settings, the diagnosis could influence whether a kid gets placed on probation or gets sent away to residential facilities.
Are these disciplinary actions in response to the label also common in white children?
Inequities related to school suspension and expulsion are particularly relevant here. Black children, and in particular Black girls, are at much higher risk of being suspended and expelled. The diagnosis feeds into those inequities.
[Related: Advocates fear students will again be subject to restraint used on George Floyd]
Certainly, white kids get punished as well, but there’s research demonstrating that white kids will often get referred to mental health treatment because their behavior is construed as something behavioral – as in they are suffering. Whereas kids of color, and in particular Black kids, it’ll be in the direction of punishment, suspension and expulsion, and eventually juvenile justice involvement.
What do mental health providers need to do different?
What the paper is trying to say is we can’t default to these existing guidelines and standards. Instead, we have to have a way of thinking about this that considers the different inequities, that looks at the way in which the diagnosis can perpetuate further harm in school, health care and juvenile justice settings. Then, we have to be primed to do something about it as part of our oath.
[Related Grant Opportunity: Improve services for youth with serious emotional disturbance]
***
Josh McGhee is the Chicago bureau chief of MindSite News and covers the intersection of criminal justice and mental health with an emphasis on public records and data reporting. He previously reported for Injustice Watch, the Chicago Reporter, DNAinfo Chicago, and WVON covering criminal justice, courts, policing, race, inequality and politics.
MindSite News is an independent, nonprofit journalism site focused on mental health, seeking to create and sustain a sense of national urgency about the workings and failings of the U.S. mental health system. Get a roundup of mental health news in your in-box by signing up for the MindSite News Daily newsletter.