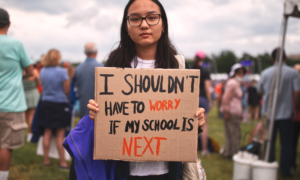
It’s flu season, and cases of asthma, diabetes and whooping cough are on the rise. At some point this winter, most children will need to see a doctor. Yet nearly 7.5 million children – one in 10 nationwide – have no health insurance, which means they’re more likely to skip that checkup or do without essential medicine.
Child advocates say the number of uninsured children is a national embarrassment, especially since two-thirds of them are eligible for subsidized medical and dental coverage through either Medicaid or the Children’s Health Insurance Program (CHIP) but have not enrolled.
Enough new children enrolled last year – more than 2.6 million – to keep the percentage of uninsured children at 10 percent, despite the worst recession in decades, rising poverty levels and a sharp decline in employer-based coverage, according to a recent study by the Urban Institute.
U.S. Health and Human Services Secretary Kathleen Sebelius has called the expansion of these programs “a tremendous accomplishment,” but also vowed, “It’s only the beginning.”
February was the one-year anniversary of legislation reauthorizing CHIP, which provides subsidized health insurance coverage for children from families with incomes of up to three times the federal poverty level. Currently the poverty level for a family of four is $20,614. Sebelius used the occasion to urge government and private-sector leaders to step up their efforts to cover even more children. “We all have a stake in America’s children, and together, we will assure that millions more get the care they need,” said Sebelius.
She and U.S. Education Secretary Arne Duncan kicked off a five-year campaign aimed at finding and enrolling the estimated 5 million uninsured children who qualify for public insurance, and Sebelius challenged federal and state officials and community-based organizations to concentrate on enrolling more of the lowest-income children.
But not every state official is enthusiastic about the expansion of Medicaid and CHIP. So far, the federal government has footed the bill for most of the expansion. Medicaid is financed jointly by Washington and the states, through a complicated matching funds formula, modified by each state’s unemployment rate.
The federal matching funds rate was increased by 6.5 percentage points in 2009, using stimulus funds, and in August, President Barack Obama provided $16.5 billion more to extend the temporary increase. But at the end of June, the formula is scheduled to revert to prior, lower reimbursement rates – even as most states face dire economic shortfalls. And some officials are already complaining about ballooning Medicaid expenses bankrupting their states.
But for uninsured families, the public safety net is a lifeline during hard times.
Health coverage equals peace of mind
Lai Lee is a refugee from Laos who emigrated to the U.S. more than two decades ago. A 38-year-old single parent, she lives in Sacramento, Calif., with her six children, five of whom are enrolled in Healthy Families, the state’s version of CHIP. Like Medicaid, CHIP is a federal-state partnership, funded largely through federally matched funds and administered by the states, which have considerable freedom to design their own programs.
Lee earns about $3,000 per month, but does not have employer-based insurance, so she pays a total of $48 in monthly premiums for her children through Kaiser Permanente. She says the subsidized coverage has been a godsend for her family. “It’s just so good to have the peace of mind, to know if something happens, I can take them to the doctor,” she says.
It’s peace of mind Lee missed in 2009, before her children were enrolled in CHIP. Her 3-year-old son Philip, who has seasonal asthma, spiked a fever of 104 degrees. She had to pay almost $1,000 in out-of-pocket costs – in advance – for doctor visits and medicine. Lee was frantic; with high housing expenses and no savings, she had to borrow money to pay the medical bills.
Even now she worries about her eldest son, Timothy. He recently turned 19 and no longer qualifies for subsidized health insurance. Last summer, Timothy suffered a head injury while playing sports at camp. He was covered then, but Lee fears what would happen if he were injured now; like many parents of uninsured kids, she tries to restrict his activities so he won’t get hurt.
Lee grew up in refugee camps in Thailand, where doctor visits were a rarity. She says children need consistent medical care in order to thrive. “For children to be happy and to learn, they have to have a healthy body and mind.”
Participation rate roulette
The odds of whether a low-income child has subsidized insurance depend largely on geography. In nearly every state, children in families with incomes up to about $45,000 qualify for public health coverage, but for the first time, the Urban Institute has documented geographic variations in enrollment. In a report released in September, Senior Fellow Genevieve Kenney found that in 2008, nationwide enrollment of children eligible for Medicaid or CHIP was nearly 82 percent. But mining state-level data, she discovered that participation rates varied widely, from 55 percent enrollment in Nevada to 95 percent in Massachusetts.
Kenney also found a concentration of unenrolled children – 1.8 million, nearly 40 percent of all eligible, but uninsured youth—living in just three states: California, Texas and Florida. Why these states? “First and foremost, because they are large states, with large populations of children,” says Kenney. “Plus, they all have larger immigrant and non-English-speaking populations, which may be a contributing factor, since we do know that kids from those families participate at lower rates.”
These populous, diverse states may pose special challenges, which, according to Kenney, provide all the more reason to focus enrollment strategies there. “You’re going to leave a major chunk of the problem unsolved if you don’t make significant progress in these large states,” says Kenney.
According to Sebelius, the new data from the Urban Institute will help direct federal outreach efforts. And new tools and resources available under the 2009 CHIP Reauthorization Act could help these populous states achieve better participation rates. “We now have a much better sense of where most uninsured children live, and which communities may need more help,” she says.
Connecting to coverage in California
Overall In California, Kenney found the public insurance participation rate close to the national average. Healthy Families, California’s version of CHIP, has nearly 876,000 subscribers. These are children from families such as Lai Lee’s, whose income ranges from 100 percent up to 300 percent of the federal poverty level (FPL). As such, they are ineligible for Medi-Cal (California’s version of Medicaid).
Children in Healthy Families have a choice of health, dental and vision plans, with monthly premiums ranging from $4 to $24 per child. The program, administered by the Managed Risk Medical Insurance Board, has a website in English and Spanish, and it accepts applications in a dozen languages, according to Ernesto Sanchez, deputy director for eligibility, enrollment and marketing. He says more than 40 percent of California applicants speak Spanish.
California’s massive budget deficit caused new enrollment in Healthy Families to be frozen for two months in the summer of 2009, and enrollment has yet to return to the pre-freeze level of about 923,000. But Sanchez has stepped up promotion strategies, which are bringing in about 25,000 new subscribers each month. He has forged partnerships with school districts, doing outreach through the subsidized lunch and school nurse programs, and handing out informational flyers at back-to-school nights.
A few months ago, Sanchez launched an outreach program through social media, with promotions through Facebook and Twitter. California also partners with 23,000 community-based organizations that act as certified application assistants – entry points where families can receive help in completing applications for Healthy Families.
Boosting coverage rates
The CHIP Reauthorization Act (CHIPRA) provided $100 million for outreach grants to promote children’s enrollment in health coverage. In April, $10 million of that was distributed to Indian tribes and their health service providers; the remaining $90 million is being awarded to states, community-based organizations and other non-profit entities as they innovate.
CHIPRA also created a new payment incentive, called a performance bonus, to encourage higher participation rates. In December 2009, Sebelius awarded performance bonuses totaling nearly $73 million to nine states that boosted enrollment beyond target levels. To qualify for the bonus, states had to adopt a range of specific measures, such as establishing a joint application for a state’s Medicaid and CHIP programs, or keeping children enrolled in CHIP for up to a year, regardless of changes in family income during that period.
Maureen Hensley-Quinn, with the National Academy for State Health Policy, says the streamlining strategies focus on easing the documentation burden. “It means cutting red tape, reducing paperwork, simplifying enrollment procedures, capitalizing on technology, and reaching out to families where they live, work or attend school,” says Hensley-Quinn, deputy director of the academy’s Maximizing Enrollment for Kids program.
Virginia, for example, has been increasing its use of technology. “Virginia now allows electronic signatures for applications,” says Hensley-Quinn. Many states have accepted online applications for years; however, parents usually were required to print out, sign, and then mail in a signature page. Program managers knew that many eligible children were being lost when their parents failed to follow through with this step. Hensley-Quinn says by shifting to electronic signatures, Virginia has virtually eliminated that problem. More recently the state has launched online renewals, which has improved its retention rate.
Alabama is piloting the use of application kiosks with language assistance technology that can translate forms or help applicants with low literacy. Other streamlining measures include dropping the requirement for an in-person interview to apply for CHIP or renew Medicaid coverage. Newborns whose mothers are already enrolled in Medicaid or CHIP are automatically eligible for coverage.
Perhaps the biggest challenge in enrolling eligible children remains spreading the word that the benefit exists. Surveys by the Kaiser Family Foundation consistently show that many low-income parents do not realize that their uninsured children qualify for Medicaid or CHIP. The surveys found that some families, especially Hispanics and Asians, may wrongly assume that their children are ineligible for coverage if a parent works, or has a car or a savings account.
According to a Kaiser survey in 2009, nearly two-thirds of Hispanic parents reported not knowing where to get information about public health insurance, and 70 percent said they did not know how to enroll their children. Yet many of these children already participate in other public benefit programs – such as subsidized school lunches – which have comparable eligibility criteria. Since the reauthorization of CHIP, states may now experiment with bypassing parents to enroll qualified kids automatically.
Express lane eligibility
One of the most useful new enrollment tools taps into existing government databases for low-income programs such as SNAP (Supplemental Nutrition Assistance Program, formerly known as food stamps) or the school lunch program. Since income criteria for these programs are fairly consistent, mining these databases is one simple way to identify uninsured children who might be eligible for Medicaid or CHIP.
This notion of “express lane” enrollment has been around for at least a decade, but it wasn’t until CHIP reauthorization in 2009 that states could apply the concept to target children who might be eligible for health insurance. Families can rely on findings from these other programs rather than resubmitting their information for health coverage.
So far at least four states – Alabama, Iowa, Louisiana and New Jersey – have been approved to use Express Lane Eligibility (ELE) to enroll Medicaid recipients.
Hensley-Quinn says Louisiana has successfully compared the names of children enrolled in its food stamp program with its Medicaid rolls, since the eligibility criteria were aligned. Without involving families in a separate application process, Hensley-Quinn says Louisiana has been able to enroll another 14,000 eligible children just since March, simply informing families of the new coverage.
These are just some of the ways that states have responded to Sebelius’ urgent call to expand health care coverage for needy children. But since she issued the challenge to cut red tape, even bigger threats to insuring these kids have emerged, including a revolt in some cash-strapped states facing record budget deficits. While many states have acted to expand their Medicaid enrollment, others are floating proposals to drop out of the program entirely.
Opting out of Medicaid
Arizona made news last month when lawmakers slashed their state’s Medicaid budget, by denying coverage for certain organ transplants. Critics accused state lawmakers of establishing de facto “death panels” for patients who could not expect to survive without lung, liver or bone marrow transplants.
Arizona had passed legislation in March repealing its CHIP statute, KidsCare – becoming the first state ever to eliminate the program. But under federal law, Arizona had to restore CHIP or risk losing $7 billion in federal matching funds. So the state never actually dropped the program. Instead, officials froze enrollment, which means families who were already covered continue to be, but new applicants were put on a waiting list, says Karen McLaughlin, with the Children’s Action Alliance in Arizona. “Since January, no new applications are being taken. Nobody’s getting in, and if you drop off the rolls for any reason, you’re gone,” says McLaughlin.
At last count, the waiting list numbered nearly 75,000, about 30 percent of whom would be denied coverage because they are ineligible, according to Jennifer Carusetta, with the Arizona Health Care Cost Containment System. Those who did qualify were enrolled in Medicaid; those who did not were referred to county-run community health care centers, which provide services on a sliding scale.
“You have to understand,” says Carusetta, “Arizona is facing an unprecedented budget crisis. Our enrollment in Medicaid has grown 30 percent since the recession. Before the end of June, we will need to identify $1 billion in order to continue funding coverage for the 1.3 million Arizonans” who receive Medicaid.
Citing similar budget woes, other states have already dropped dental benefits from Medicaid coverage; others are limiting diagnostic tests and coverage for physical therapy.
The most drastic cost-cutting steps would spell the end to any coverage at all. So far, officials in five states—Washington, Texas, South Carolina, Wyoming and Nevada—have publicly flirted with scrapping their state Medicaid programs by 2014, when many provisions of health care reform kick in. Lawmakers in those states have proposed either shifting the burden of insuring low-income children to the federal government, or funding a much more limited alternative entirely through state funds.
The most outspoken proponent of shifting the burden to the federal government has been Gov. Rick Perry (R) of Texas. Citing his looming budget deficit, Perry has pointed to research from the Heritage Foundation, which found that Texas could save $46.5 billion by dropping Medicaid and pushing low-income residents into federally subsidized insurance exchanges.
Texas Health and Human Services Commissioner Tom Seuhs declared that Medicaid needs to be “reinvented,” as his agency released a report showing that the expenses for more than half of all births in the state are paid for by Medicaid. Dropping the program could affect as many as 2.6 million Texans, according to the state report.
Despite such proposals, health care reform advocates aren’t too worried that Medicaid is seriously threatened. “I think we need to take that for what it is right now, which is largely politically motivated talk,” says Jennifer Sullivan, senior health policy analyst with Families USA. “Very few states would walk away from the kind of federal money that’s on the table through Medicaid; it’s not a risk many states would be willing to take.”
Public solutions don’t reach everyone
Even if public insurance programs survive, and even if Medicaid and CHIP succeeded in enrolling every eligible child, 2.5 million other youth would still be out of luck. These are children whose family income is too high to qualify for government-subsidized care, yet they have no private coverage. In most cases, their working parents have no access to employer-sponsored health insurance and cannot find or afford coverage in the individual market.
Some relief for them may be coming through the Affordable Care Act, which mandates that children on private insurance may not be denied coverage because they are sick. Beginning in September, the health care reform law required all insurers to accept children regardless of their pre-existing conditions. A number of insurers – including WellPoint, UnitedHealth Group, Aetna, Cigna and Humana – reacted to the new rules by withdrawing from the market for “child-only” policies. Carriers complained that these policies had become too risky, since parents could wait until a child became sick and then demand coverage.
But some states fought back. Washington, Oregon and California passed emergency rules or enacted legislation requiring all insurers selling individual insurance to provide child-only policies, at least during limited open enrollment periods. Colorado succeeded in luring two insurers back into the market by also restricting when children had to be accepted. Sebelius reports she is working with other carriers to restore the market for child-only coverage.
Another problem looming in the private market: Some health insurance funds are dropping coverage for children enrolled in group policies. In October, a fund administered by a New York affiliate of the Service Employees International Union announced that starting Jan. 1 it would deny coverage for dependents of its members—more than 30,000 low-wage healthcare workers.
A total of 6,000 children could lose benefits, according to union spokesman Mitra Behroozi, who said the fund faced a $15 million shortfall for 2011 because of increases in insurance premiums. In a statement, Behroozi also blamed the federal health care law for requiring insurance plans with dependent coverage to extend that coverage up to age 26. Behroozi claimed the expansion, in September, had also resulted in big rate hikes.
So, despite some progress on the public side, the coverage gap for children remains. Despite the widely shared goal of ensuring that all children have access to high-quality medical care, that gap is likely to persist into the next decade.