Improved access to treatment is a vital step toward addressing the rising tide of opiate addiction. Scientific advances that support the disease model of addiction, together with changes in epidemiology, have shifted public sentiment and led to a policy focus on treatment and prevention more than ever before.
Improved access to treatment is a vital step toward addressing the rising tide of opiate addiction. Scientific advances that support the disease model of addiction, together with changes in epidemiology, have shifted public sentiment and led to a policy focus on treatment and prevention more than ever before.
President Barack Obama recently proposed expanding evidence-based treatment programs in an effort to lower the bar for patients to enter effective treatment programs. The resources put into treating patients with substance use disorders are well spent.
However, opioid addiction is the culmination of a process of drug exposure, typically beginning in adolescence, that results in neurological changes in the brain that can be managed, though not cured. While treatment is critical, prevention is the only way to truly interrupt the epidemic of opiate addiction.
Indeed, the Adolescent Substance Abuse Program at Boston Children’s Hospital has yet to treat the opiate-addicted patient whose substance use history did not begin with alcohol and/or marijuana use. In fact, individuals who use marijuana before age 17 are four times more likely to develop opioid addiction.
During the past 12 years there has been a substantial drop in the overall rates of substance use among teens. This is in the context of a vigorous public health campaign to engage health care providers to ask about and address substance use via evidence-based tools used in a framework called Screening, Brief Intervention, Referral to Treatment, or “SBIRT.”
In pediatric settings where children and teens receive health care before they start using substances, SBIRT can target prevention. Evidence suggests that brief interventions can delay and reduce alcohol use by teens.
Even small delays and reductions in use can have massive public health implications because adolescents are exquisitely susceptible to both acute and long-term consequences of exposure to psychoactive substances. For example, the growing adolescent brain is uniquely vulnerable to developing the neurological changes of addiction; indeed, the large majority of adults in substance use treatment started using prior to age 18.
[Related: How Young Peers in Recovery Are Amplifying Prevention and Early Intervention]
Discussing substance use openly and honestly with adolescents can do much more than slow the stream of addiction. Even among those who never develop a substance use disorder, alcohol and other drug use account for the vast majority of life-years lost due to disease, disability and premature death among those aged 15 to 24.
Introducing substance use as a legitimate topic for health care discussion before use starts may shape attitudes today and open the door to more complex discussions during the teen years and beyond. The return on investment is likely to be considerable given the potential for lifelong savings in health care dollars and in suffering.
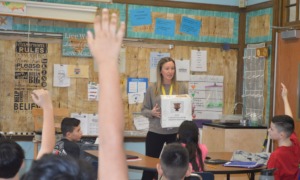
Yet delivery of SBIRT solely within health-care settings is inefficient. Adolescents have the lowest utilization of primary care of any age group. To turn the tide on opiate addiction and right the course of many young lives before intensive and costly treatment is needed, we need to take early detection and brief intervention to school, the setting youth most often frequent and an ideal context for holding a caring and confidential conversation with a trained professional.
School nurses provide a viable and willing workforce for undertaking this: They are already on the front lines of addressing youth substance use and need tools, training and state support.
We cannot afford to waste time when so many lives — including young lives — are at stake. An ounce of early, brief intervention today is a sound and timely investment when measured against the many pounds of effort required to try to treat our way out of this problem tomorrow.
Sharon Levy, MD, MPH, is the director of the Adolescent Substance Abuse Program at Boston Children’s Hospital and an assistant professor of pediatrics at Harvard Medical School. Julie Lunstead, MPH, works at the Adolescent Substance Abuse Program at Boston Children’s Hospital. And Elissa R Weitzman, ScD, MSc, is on the faculty for Adolescent/Young Adult Medicine at Boston Children’s Hospital and is assistant professor of pediatrics at Harvard Medical School.
More related articles:
Talking to a Doctor About Substance Use