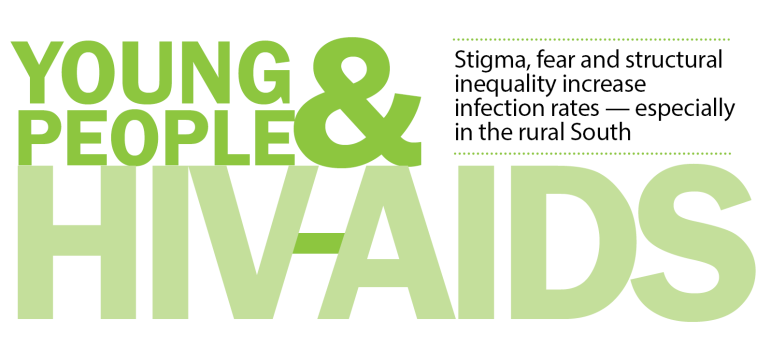
 ATLANTA — The number of HIV-positive cases among 13- to 24-year-olds is increasing at alarming rates, according to HIV and AIDS researchers, with youth and young adults accounting for 26 percent — or 12,200 cases — of all new HIV infections in the United States in 2012.
ATLANTA — The number of HIV-positive cases among 13- to 24-year-olds is increasing at alarming rates, according to HIV and AIDS researchers, with youth and young adults accounting for 26 percent — or 12,200 cases — of all new HIV infections in the United States in 2012.
In Atlanta, the percentage of new HIV infections in that age group is almost double, with 50 percent of new HIV infections occurring in 13- to 24-year-olds, according to The Community Foundation for Greater Atlanta. In contrast, 13- to 24-year-olds make up 17 percent of the U.S. population, according to figures from the Centers for Disease Control and Prevention (CDC).
And while most of the new infections occur in metropolitan areas, there’s now a new twist that concerns public-health officials.
HIV and AIDS researchers are concerned about an uptick in HIV among youth in some rural areas, almost all in the Deep South, including North Carolina, South Carolina, Georgia, Florida, Tennessee, Alabama, Mississippi, Louisiana and Texas. Those same researchers say lack of access to preventive health care and lack of outreach and education in rural areas put poor, rural youth and young adults at heightened risk.
Stigma and fear
“I think all the things overlapping — race and socioeconomics, education, access — all play a role” in the increased HIV infection rates in rural parts of the South, said Dr. Travis Sanchez, a professor of public health at the Rollins School of Public Health at Emory University in Atlanta and the lead researcher on new data recently released on HIV incidence.
[module type=”aside” align=”right”]Nearly 60%
Percentage of HIV infection is higher in the Deep South states than for the United States as a whole. The rate for the Deep South is 10.6, compared to 6.2 for the entire country.
Journal of Community Health, 2014
23.3%
Percentage of cases in the Deep South that are youth between 13 and 24. The national average is 21.6.
Journal of Community Health, 2014
77%
Percentage of all new AIDS cases in Georgia represented by African Americans even though they make up only 29 percent of Georgia’s population.
The Community Foundation for Greater Atlanta
It is also important to consider the role that stigma and fear play in the prevention, early detection and effective treatment of HIV among rural residents, said Dr. Patrick O’Neal, director of health protection for the Georgia Department of Public Health.
“The stigma against HIV in rural areas tends to be different than in metro areas,” said O’Neal.
Cases of HIV in rural areas in Georgia are most likely to occur in African American men having sex with men — and many of them are young men and teens, O’Neal said.
“Many gay individuals are closeted, and they don’t let anyone know,” he said. “They may travel into a metro area, have sex, return home and never talk to anyone about it.”
The secrecy feeds stigma, he said.
“The stigma of men having sex with men (in rural areas) is great,” O’Neal said. Religious fundamentalism, which often condemns same-sex relationships, and familial disapproval of same-sex relationships make it difficult for gays and lesbians in rural areas to be themselves sexually — and to seek and practice health care that is appropriate for their lifestyles, O’Neal said.
“There are great concerns that we need to do a better job addressing the stigma,” O’Neal said, explaining that stigma prevents people from getting tested for HIV early and for getting treatment.
And while prevention programs are great, O’Neal said messaging about early detection, treatment and a strict adherence to treatment might be even more important to stem the rise of HIV in rural areas.
“We’ve entered an interesting phase, where the best prevention is early treatment,” O’Neal said. “We can reduce transmission by 96 percent with effective treatment [using anti-retroviral drugs].”
In contrast, condom usage reduces transmission by 80 percent, O’Neal said.
Yet getting people in the rural South to go to a local clinic for help is difficult.
“They don’t want to come into clinics,” O’Neal said. “They want to be treated by a family doctor.”
Emily Brown, field coordinator with Georgia Equality and former manager of HIV research projects at Emory’s Rollins School of Public Health, said that many newly diagnosed people — be they young, middle-aged or older, do not want to seek help at all.
“It’s easier in some ways to stay in denial,” Brown said.
That, of course, worsens a person’s health — and spreads the disease.
“They may have great fear, and how do we help people who have this terrible fear? How do we break through all that?” O’Neal said.
Structural challenges to address
As challenging as it is, the increased incidence of HIV cases in rural areas may provide insight and information into the overall increase, because it may also provide clues about structural problems — such as lack of access to health care, homelessness, poverty, lack of education — that contribute to the overall rise of HIV cases.
“There’s definitely something different about the prevalence in the South,” said Sanchez.
“There are really high rates compared to how big the counties are. In some, they are at rates similar to what we’d see in big cities.”
The South in general — and not just its rural areas — is the most heavily affected area by HIV and AIDS, Sanchez said.
“When we rank the 10 highest cities, seven or eight of them are in the South,” he said.
And, now, most of the highly affected rural areas are in the South, too, with more rural counties showing increases in HIV cases in males ages 13 to 24 than any other U.S. region.
Also, a 2014 article published in the Journal of Community Health showed that prevalence of HIV infection in the Deep South states is nearly 60 percent higher than for the United States as a whole. The rate for the Deep South is 10.6, compared to 6.2 for the entire country.
And, 23.3 percent of those cases in the Deep South are youth between 13 and 24, compared to the national average of 21.6.
[module type=”aside” align=”right”]26%
Percentage of all new HIV infection rates (or 12,200 cases) in 2012 that were among 13- to 24-year-olds.
[/module]Sanchez said that data show that the trend in these areas is upward, not down.
“The pattern’s been known for quite awhile,” Sanchez said. “It probably overlaps with race and socioeconomics, education, access.”
Brown echoed that “structural inequality” is behind the increases, not “risky behavior.”
“It’s more about the ways our society does not serve people at risk,” Brown said. The data indicate that most of the new cases of HIV are African American in Georgia and the nation, continuing a decadeslong trend in which the virus takes a much more severe toll on African Americans.
“African Americans in general have poor access to health care, have fewer access points and are victimized throughout life,” Brown said. African Americans, who make up 29 percent of Georgia’s population, represent 77 percent of all new AIDS cases in Georgia, according to the Community Foundation for Greater Atlanta.
Poverty is ultimately the driving factor for all of it, Brown said.
“HIV is always a contextual issue,” Brown said. “It’s a canary in a coal mine for inequality.”
And the effects of rural poverty are playing out across the South, with leaders struggling for ideas that would lead to solutions.
John Rogers, an HIV educator for 10 rural Georgia counties in the far southern part of the state, said the majority of people who are HIV positive with whom he works are very poor. If they are older than 18, they do not have insurance, because the state chose not to expand Medicaid to the very poor.
“Many of them have issues that are more pressing than their HIV,” he said. “They don’t have housing. They don’t have a job. And they may have more important health issues that they need to take care of before they address their HIV.”
Reaching them is difficult not only because they are poor but also because of powerful stigma in small rural towns and counties.
“They don’t want to identify as HIV positive because then they would in essence out themselves. And that would complicate their lives even more,” said Rogers.
A sore spot
O’Neal said the Georgia Department of Public Health has ideas and programs in place that would help. For example, through a grant from the federal government, Georgia has recently begun a program that allows a doctor in Atlanta to connect via telemedicine to many sites across the states.
But advocates said they realize that more needs to be done. Georgia, like many of its neighboring Southern states, is in the middle of a crisis with its rural hospitals. Many are on the verge of collapse, and several have closed in recent years. The closing of rural hospitals and the shortage of pediatricians and other primary-care doctors in rural parts of Georgia and other Southern states show the challenge of meeting even basic health care needs. That in large part is due to low Medicaid reimbursement rates: Doctors have said they cannot afford to practice in counties that have a high percentage of Medicaid patients. In many rural counties, as many as 75 percent of residents are on Medicaid, according to figures from Georgia’s Department of Community Health, which administers Medicaid in the state.
[module type=”aside” align=”right”]Resources
If you want to provide info to teens you serve, or educate yourself on the matter:
- AIDSVu, created by the Rollins School of Public Health at Emory University in partnership with Gilead Sciences, Inc., offers interactive U.S. maps showing infection rates as well as testing and care sites.
- The CDC publishes fact sheets, offers an interactive map for searching testing sites by ZIP code, and a dozen other resources online.
- Greater than AIDS offers a “public information response to the U.S. domestic epidemic.” Supported by a broad coalition of health service providers, funders and activists, this site offers information about insurance coverage, testing, advocacy and more at the national and local levels. It also offers its site and resources in Spanish.
With few doctors and with community health departments stretched thin in rural counties, access is affected, Brown said. That could explain a related problem: getting youth to stay compliant with treatment regimens after they are diagnosed.
“Only 30 percent of youth are actually taking their medications, and that has to do with access to care,” Brown said, citing figures from the Georgia Department of Public Health.
Combating the surge is difficult, Brown and others said. Information efforts are small, often no more than a link on a website.
Yet educating young people about HIV and reaching those who need to be tested are vital to combating the spread of the virus. Brown said doctors should be testing for HIV in all patients. In Georgia, youth 13 and older can be tested without parental consent, she said.
“As a service organization, it’s incumbent to seek out teens for testing,” Brown said. “And to educate. They’re not getting it at school.”
An even bigger problem arises when someone finds out he or she is HIV positive, Brown said.
“It’s a big leap to find out you’re positive and then to actually take your medicine,” Brown said.
Doctors and others who treat young patients in rural areas might not have solid plans on how to get an HIV positive youth to return for follow-up appointments.
“It’s a sore spot,” she said. “It’s frankly very difficult to track down somebody who’s trying to survive.”
See sidebar “From the Field: Youth-led HIV & AIDS Awareness Day” and watch for a multimedia package coming next week.