If you ask people what type of disease is most prevalent in children, few would say dental disease. But tooth decay is the “single most common chronic childhood disease – five times more common than asthma and seven times more common than hay fever,” according to the U.S. Surgeon General’s 2000 report, “Oral Health in America.” 
Twenty-five percent of youth have untreated tooth decay, according to a 2000 U.S. Government Accountability Office (GAO) study.
As with many health problems, poor kids are the most likely to suffer from ailments and lack of treatment. Almost 80 percent of tooth decay in poor children is untreated, according to the GAO.
The problem isn’t just in little kids with candy-driven cavities. A lot of dental problems result from injuries, such as getting hit in the mouth while playing sports. And “tobacco-related oral lesions are prevalent in adolescents who … use smokeless (spit) tobacco,” the surgeon general’s report said.
“To us, the most pressing issue is a question of equity in oral health and access to dental care,” says Burton Edelstein, founder of the Children’s Dental Health Project, a nonprofit health advocacy organization based in Washington.
Aside from the pain and complications of cavities, discolored teeth and sore gums, dental problems can impair speech development and interfere with a youth’s focus in class, said a 1998 report from the National Maternal and Child Oral Health Resource Center. The 2000 U.S. Surgeon General’s report estimated that children miss 51 million school days each year because of poor oral health.
Many oral health problems are actually easy to address, say pediatric dental experts, but when left unattended, they can have devastating results. Regular visits to a dentist can prevent decay through such basic measures as cleaning teeth and treating them with fluoride, while most tooth and gum damage is reversible with proper care.
Sealants, which are applied by dentists to prevent cavities, provide another line of defense. “Sealants are especially important for kids with poor access to dental care, because they may prevent tooth loss later in life,” says Doug Foster of the Tillman Dental Clinic, a government-funded facility that serves indigent youth in El Paso, Texas.
But how many youth-serving agencies have dental equipment, much less staff who are trained in how to use it?
The good news is that the State Child Health Insurance Program (SCHIP) is making progress in meeting dental demand, while some youth-serving agencies are using creative alliances to meet the needs of poor youth as cheaply as possible.
A study of 27 state SCHIP programs by Mathematica Policy Research – “SCHIP Takes a Bite Out of the Dental Access Gap for Low-Income Children,” released last month – found that most of the states have already reached or exceeded the program’s goal of providing 57 percent of low-income children with dental services by 2010.
In states that are falling short or do not include dental services in their SCHIP programs, youth programs work to plug the gaps. Some have used partnerships with university dental schools or with major youth programs like Boys & Girls Clubs. Others use low-cost models to bring services to low-income rural and immigrant youth.
Following are descriptions of four programs that provide dental care to underserved youth.
Youth Agency Partnership Carilion Dental Care – Pediatrics 101 Elm Ave. Roanoke, VA 24017 (540) 224-4380 www.carilion.com/pediatrics/html/dental.html
Every Thursday, staffers from the Boys & Girls Clubs of Southwest Virginia load kids onto a bus and drive them to a place that most people dread: a dentist’s office.
“It was literally pulling teeth to get kids to participate at first,” admits Executive Director Becci Emanuelson.
But the partnership among the club, Carilion Health System and Delta Dental Plan of Virginia has paid off for everyone, especially the children. Called Smart Smiles, the program gets underserved youth to the dentist on a regular basis, and makes it appealing.
The clinic was born of frustration. Local youth service agencies and community health leaders had explored several options to increase poor youths’ access to dental care. That included lobbying for increases in Medicaid reimbursement and enlisting local dentists to accept five underserved children each per year. Both efforts met with limited success, so the advocates set out to fund a pediatric dental clinic.
“Raising $1million was the easiest thing we did,” says Bud Conklin, medical director for Carilion Dental Care in Roanoke, Va. Virginia Health Care Foundation, the Carilion Community Health Fund and the Maupin-Sizemore Foundation provided start-up grants to help Carilion open a state-of-the art facility.
The biggest hurdle, says Conklin, was recruiting a pair of “scarce as hen’s teeth” pediatric dentists to serve children under 12. Carilion Dental Care – Pediatrics opened in April 2001 to provide comprehensive oral health services to medically, physically, developmentally and financially underserved children.
The clinic was nearly overwhelmed by its initial success. Many patients arrived with severe needs like abscessed teeth, and most had never seen a dentist. The clinic worked its way through the influx by employing a second dentist.
The initial plan was to serve kids eligible for Medicaid and FAMIS (Family Access to Medical Insurance Security), but the partners realized that transportation can be a barrier for all children. So they opened the doors to those with private insurance. About 15 percent of Smart Smiles participants are privately insured, which may help reduce any stigma associated with participating in the program.
The clinic serves nearly 8,000 of the estimated 63,000 local children living at or below the poverty level. Some 700 kids and their families are enrolled in the clinic’s Smart Smiles partnership with the Southwest Virginia Boys & Girls Club.
Every Thursday, Carilion books 18 appointments at the clinic for Smart Smiles patients. Delta Dental Plan of Virginia, an insurance company, provides the bus. The clinic needs a high patient volume to break even, and such block scheduling helps, because it reduces the number of no-shows.
The youths get T-shirts and toothbrushes. The collaboration extends beyond cleanings and fillings, with partners reinforcing educational messages. Dentists and assistants handle one-on-one education, lecturing on brushing habits and the woes of tobacco and soda. The club taps into Delta Dental’s Teeth on the Go and Crest Cavity Free programs for hands-on lessons in brushing and flossing. Kids at the club use papier-mâché to fill mock cavities and reduce fear and anxiety.
The clinic is self-sustaining: Medicaid pays for 92 percent of its patients, Carilion covers overhead costs, and Delta Dental pays for Smart Smiles patients without coverage.
Carilion is trying to raise $1.5 million to expand its facilities and hire more staff, including someone who can handle more complex cases in teens. Plans are to expand Smart Smiles throughout Virginia. The Virginia Healthcare Foundation has declared the program “a model that made it” and hopes to help other organizations replicate it.
Medical Partnership Centro San Vicente Dr. Jaime Martinez Dental Clinic 8061 Alameda Ave. El Paso, TX 79915 (915) 859-7545 www.sanvicente.org
While lack of dental care is a near-universal problem among poor children, recent data indicate that noncitizen and Hispanic children are disproportionately affected. Nearly half of such children in a recent survey had no preventive visits to the dentist in the previous year, compared with 26 percent of their low-income peers, says Genevieve Kenney, principal research associate with the Urban Institute.
In the late 1990s, Community Voices El Paso tried to narrow that gap by paying local dentists to provide dental care and oral health education to uninsured and underinsured families. The plan hinged on a $77,000 Kellogg Foundation grant, but the money couldn’t be used to pay for services – forcing Community Voices to find another way.
The grant could, however, be used to equip a provider to serve the community. Enter Centro San Vicente, a health clinic that already had plans to add a dental clinic. The organizations teamed up and pursued more grants, as well as private donations, raising $150,000 to purchase equipment and open the Dr. Jaime Martinez Dental Clinic last August.
The dental clinic is located at the main facility, which provides an array of health services for local families. The set-up enables Centro San Vicente to link pediatric care with dental care at one location: Pediatricians screen children for dental needs and refer them to the on-site dentist as needed.
Centro San Vicente Executive Director John Romero believes its impact with kids might be strengthened by the fact that it serves entire families. “Parental involvement could strengthen the behavioral aspects of oral health,” Kenney agrees. But she cautions that sometimes it’s best to approach youth directly. For example, when parents have mental health problems, they are less likely to pursue dental care for their children.
Centro San Vicente pays close attention to language and cultural issues as well as family dynamics. Health educators host one-on-one and formal classroom preventative programs in Spanish and English. One of their major efforts is preventing baby bottle caries, which results from letting babies sip sweetened juice and soda from bottles. Educators show parents graphic examples of the results of the practice and suggest practical alternatives.
Educators also tout the new dental services in general education programs and at health fairs, recruiting new patients. “We get a multiplier effect with these programs, because we keep them family-oriented and open entry,” says Romero. Patients bring extended family members and friends, who then tap into the clinic for care.
A mere 18 percent of the clinic’s patients are covered by Medicaid, and the majority lack insurance. Centro San Vicente aims to offer affordable dental care by pegging fees to 25 percent of customary charges. It survives on fees, private donations and federal grants, such as grants from the Department of Health and Human Services to provide care to underserved populations. So far, about 20 percent of the dental clinic’s patients are youth, but Romero aims to increase that figure with several initiatives. In February, the clinic hosted Give Kids a Smile Day. More than 200 children received free screenings, cleanings, fluoride treatments and sealants, as well as educational materials. In keeping with its emphasis on health education and family involvement, parents had to participate in a mandatory pre-screening two weeks before the visit.
The clinic also plans to target local schools, Head Start programs and youth-serving agencies.
University Partnership The Children’s Dental Center 260 East Buckthorn St. Inglewood, CA 90301 (310) 419-3000 www.toothfairycottage.com
While funding is typically cited as the most daunting challenge for getting dental services to underserved youth, The Children’s Dental Center (TCDC) has come close to a solution.
Its keys to financial stability are that it was founded by a nationally known dentist, Dr. Cherilyn Sheets, and it works in partnership with a university.
Sheets is the daughter of Dr. James B. Sheets, a local dentist who reportedly accepted baked goods in exchange for services from some low-income families.
In 1988, when the elder Sheets retired, his daughter continued his dental practice and took his charitable tradition further. She opened TCDC in 1995, teaming with the University of Southern California (USC) School of Dentistry, and serves as chairman of the board.
Its mission, as described by Development Director Lisa Daggett: “education and oral health care for children who are economically disadvantaged but with working parents.”
The program is carried out in two buildings: the Smile Store, where youth receive treatment, and the Toothfairy Cottage, a comprehensive educational center built into the Sheets’ family home across the street.
Each child who visits is required to attend educational sessions with a parent. The youths learn proper oral care, and are taught about nutrition and the effects of sugar through fun exercises, such as seeing the amount of sugar in a can of Coke. Young children, many of whom are making their first visits to the intimidating dental chair, play dentist to alleviate their fears.
The hope is that the youths “develop the capacity and skills to become genuine partners” in their oral health, says Dr. Steven Uranga McKane, executive director of TCDC.
Each year about 5,000 children, ages 2 to 18, qualify for services. Their parents must be working, and the family income must be below 250 percent of California’s poverty line.
Because they serve the working poor of Southern California, many of whom speak Spanish, the staff must be bilingual. The patients pay $25 per visit, compared with about $127 in a local private practice. Significant procedures such as major surgery are not covered by the $25 fee, but they are still priced below market. Root canals, for example, range from $125 to $175 for up to three teeth.
Parents who cannot afford the fees can instead volunteer in the center or the Toothfairy Cottage. Contributions from groups such as Discus Dental, the National Dental Network and Patterson Dental Co. help cover the costs. The notoriety of the Sheets family brings in donations from colleagues, professionals who went to dentistry school with Sheets or her father, and admirers from other states. The program has a $1.2 million budget this year, with $925,000 of that projected to come from contributions, according to the center.
The partnership with USC helps to keep down costs. Students at USC’s School of Dentistry hone their skills and complete off-campus learning experiences through TCDC.
Daggett doesn’t rest on the solid financial footing. “You can’t ever take your funding stream for granted,” she says.
Going Mobile University of Rochester Community Dentistry 625 Elmwood Ave. Rochester, NY 14620 (585) 273-1953 www.urmc.edu/dentistry/education/comm_den_odp.cfm
Sometimes, the best way to reach kids is to meet them on their turf. The University of Rochester Community Dentistry SMILEmobile has done just that since 1967, when the Monroe County Dental Society and Eastman Dental Center set out to care for underserved youth in the city and in Rochester’s outlying rural areas.
Each of the three SMILEmobiles is a full-service dental trailer that parks next to schools for three to six weeks of intensive dental care. A complete staff – dentist, hygienist, dental assistant and administrative coordinator – provides preventative and basic services, including oral exams, X-rays, cleanings, fluoride treatments and sealants. Referrals for specialty services like space maintainers are coordinated among the university’s Pediatric Dentistry Program, Eastman Dental Center and local dentists.
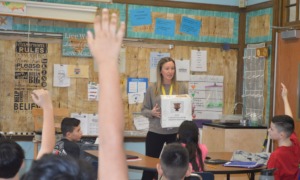
The mobile units rotate among 14 elementary schools in the Rochester area, serving 2,250 children a year. What program administrators do not want to do, however, is provide six weeks of care and go away. That’s why the community dentistry department sets up an oral health education program in participating schools. Various grade-level curricula address oral care basics, while the RAP/Jingle-Rhyme program encourages students to develop oral health poems, illustrations and songs, which are often shared in school-wide assemblies.
Starting in 1995, the department also bought portable dental units for seven satellite sites. (They’re less expensive than SMILEmobiles, which run $250,000 to $275,000 apiece.) The sites, primarily schools and health centers, are selected based on the number of low-income families in each area. Each satellite is staffed with a dentist, hygienist, assistant and administrative coordinator.
“Quite often, the dental needs of the rural community are greater than those of the urban,” explains Holly Barone, senior operations administrator for the university’s Community Dentistry and Oral Disease Prevention program. Many rural communities are not fluoridated, which can increase dental decay. Outlying Livingston County has no dentist who accepts Medicaid, forcing underserved families who have reliable transportation to drive about 50 miles to Rochester for care.
That’s why the program brings SMILEmobiles to rural communities in the summer. In the 1990s, the program combined grants from the Rochester Primary Care Network and the state to set up a satellite clinic and portable dental units in Livingston County. In all, the community dentistry program completes more than 22,000 patient visits each year (youth and adults) at rural outreach sites.
The department’s funding sources include Medicaid; federal, state and county grants and contracts; individual and corporate donations; and grants from foundations such as the Aetna Foundation and Ronald McDonald Charities. Some satellite clinics charge a sliding scale fee to serve youth who are not covered by Medicaid, while SMILEmobiles provide free care to youth referred by school administrators or social workers.
In the department’s latest outreach effort, more than 20 dentists have been recruited as partners to increase access among underserved, uninsured and homeless children and adults. In exchange for competitive stipends, the private-sector dentists provide services in the satellite sites and mobile units.